Introduction to Universal Healthcare
Universal healthcare refers to a system that provides healthcare services to all individuals, regardless of their socio-economic status, geographical location, or pre-existing health conditions. This concept is built on the fundamental belief that access to healthcare is a basic human right and essential for the overall well-being and productivity of society. It aims to ensure that everyone has access to necessary health services without experiencing financial hardship. The critical aspects of universal healthcare focus on three main principles: equitable access to health services, affordability, and quality of care.
Equitable access signifies that all members of society can obtain healthcare services without facing barriers, such as high costs or limited availability. This principle actively seeks to eliminate disparities in healthcare access, ensuring that vulnerable populations are prioritized and receive the necessary attention and resources. Affordability refers to the aspect of financial protection; universal healthcare systems are designed to minimize out-of-pocket expenses, which can often lead to individuals avoiding necessary medical care. The goal is to create systems where the financial burden of healthcare is managed through public funding or insurance schemes rather than directly by the patients themselves.
The quality of care encompasses not only the availability of services but also the standard of those services provided. Universal healthcare models strive to maintain high-quality healthcare, which is essential for achieving favorable health outcomes in the population. By integrating preventive, primary, and specialized care, these systems work to address health issues proactively rather than reactively.
Ultimately, universal healthcare has profound implications for individual well-being and societal health. It promotes healthier populations, reduces inequalities, and enhances protective health measures, contributing to the overall stability and economic growth of nations. This introduction sets the foundation for examining various universal healthcare models globally and their impacts.
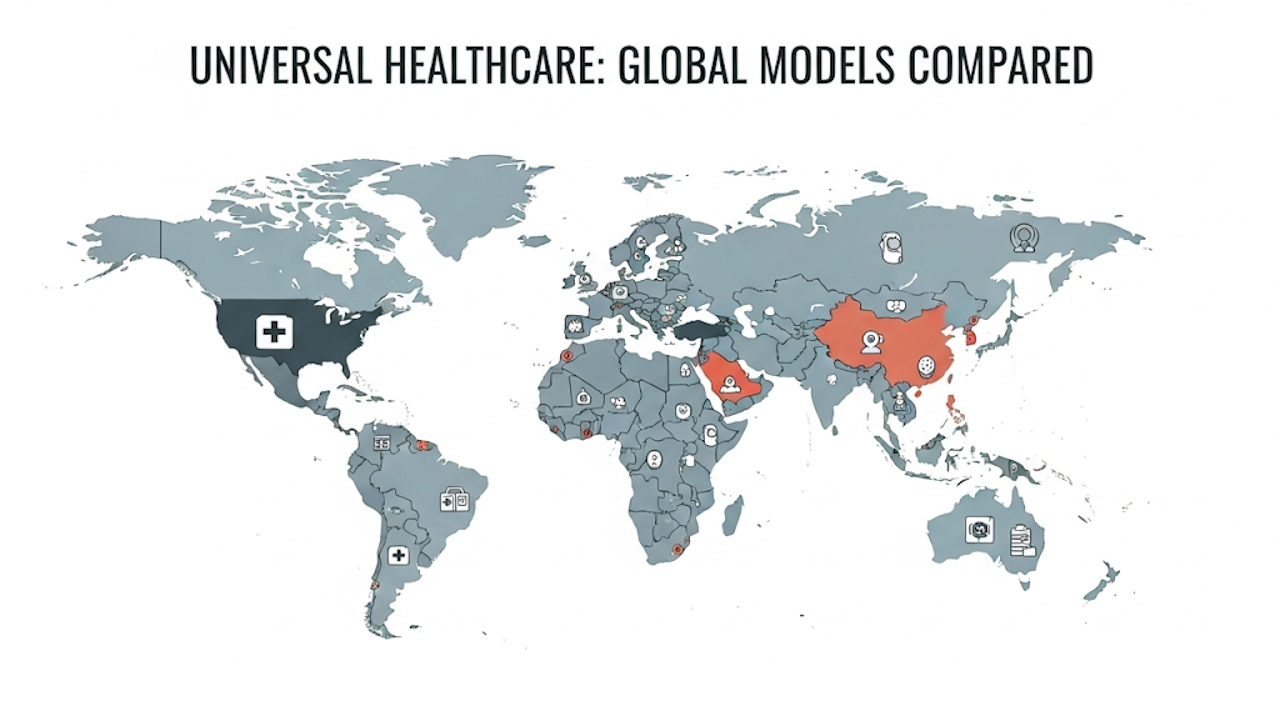
Models of Universal Healthcare Around the World
Universal healthcare has become a pivotal topic in global health discussions, with various countries adopting distinct models to ensure health coverage for their populations. These models can broadly be categorized into three primary types: the Beveridge Model, the Bismarck Model, and the National Health Insurance Model, alongside several hybrid systems proving effective in certain nations.
The Beveridge Model, exemplified by the United Kingdom, is funded by taxation and offers healthcare services directly provided by the government. In this system, healthcare is free at the point of use, ensuring that citizens do not face financial barriers when accessing medical services. The government controls healthcare costs and services, allowing for a regulated system that prioritizes public health outcomes, although critics often point to potential limitations in resource allocation and long wait times for services.
In contrast, the Bismarck Model, as implemented in Germany, relies on a dual system of funding through employee and employer contributions to non-profit insurance organizations. This model allows for a high degree of choice among providers and ensures comprehensive coverage. The German system has shown effectiveness in managing costs while providing high-quality healthcare services. However, it may present challenges related to insurance administration and navigating multiple providers, which can complicate the overall healthcare experience.
The National Health Insurance Model, represented by Canada, combines elements of both the Beveridge and Bismarck models, using taxation to fund a government-administered insurance program. This model ensures all residents have access to medically necessary healthcare services without user fees at the point of care. However, certain services, such as dental and vision care, may be excluded, leading to debates about the comprehensiveness of this model.
Hybrid systems, such as those in Australia and the Netherlands, blend elements of these models to leverage their strengths while minimizing weaknesses. Australia’s Medicare system exemplifies a mix of public and private sector involvement, allowing for both state-funded healthcare and private insurance options. Similarly, the Netherlands mandates private insurance for all residents, with extended public oversight to ensure comprehensive coverage. Through these diverse models, countries continue to strive toward delivering universal healthcare, adapting mechanisms according to the needs of their populations and the unique challenges they face.
Benefits and Challenges of Universal Healthcare
Universal healthcare systems present a myriad of advantages and disadvantages that are critical to understanding their overall effectiveness. One of the primary benefits is the improvement in health outcomes across populations. Access to healthcare services without the barrier of prohibitive costs allows individuals to seek medical attention promptly, which can result in earlier diagnoses and improved management of chronic conditions. Additionally, universal healthcare can lead to a reduced financial burden on individuals. By distributing healthcare costs across the entire population, it mitigates the risk of medical bankruptcy, allowing families to allocate their resources more effectively toward other essential needs.
Moreover, enhanced preventive care is a significant advantage of universal healthcare. When access to healthcare is available to all, there is a greater emphasis on preventative measures such as vaccinations and routine screenings. This not only serves to improve general health but can also reduce the long-term costs associated with treating advanced diseases. These benefits illustrate how universal healthcare systems can contribute positively to public health and economic stability.
Conversely, universal healthcare systems also face notable challenges. A primary concern is the sustainability of funding. Ensuring that the system remains financially viable requires careful planning and significant investment from governments. Without adequate funding, the quality of care can deteriorate, leading to dissatisfaction among citizens. Another challenge is the potential for increased wait times for medical services, as demand may outstrip available resources in certain regions. This can result in delays for patients seeking care, which can have negative implications for health outcomes.
Furthermore, issues of quality and efficiency arise when a universal healthcare system is unable to balance the demand for services with the supply of healthcare providers and infrastructure. Striking a balance between accessibility and quality remains a central challenge for many countries implementing universal healthcare. Understanding these benefits and challenges is essential in assessing the effectiveness of universal healthcare models globally.
The Future of Universal Healthcare: Trends and Innovations
The evolving landscape of universal healthcare is marked by various trends and innovations that show promise for the future of global health systems. One key area of transformation is the integration of technology into healthcare delivery. Advancements in digital health, such as electronic health records and health information exchanges, facilitate better coordination of care and enhance patient engagement in their health management. By harnessing data analytics and artificial intelligence, healthcare providers can make informed decisions, leading to improved patient outcomes and increased efficiency within systems.
Telemedicine stands out as a significant innovation in the future framework of universal healthcare. The COVID-19 pandemic catalyzed its widespread adoption, allowing patients to receive care from the comfort of their homes. This mode of delivery has proven especially beneficial in rural and underserved areas, bridging gaps in access to healthcare services. Telehealth not only reduces barriers to care but also emphasizes the need for continuity in health service delivery, ensuring that individuals receive timely interventions without the necessity of physical visits to healthcare facilities.
Another crucial aspect of future universal healthcare systems is the integration of mental health services into overall healthcare provision. Acknowledging the relationship between mental and physical health has gained traction in recent years. Policymakers are increasingly recognizing that mental health cannot be treated in isolation; thus, innovative models are emerging that promote holistic well-being and comprehensive care. This integrated approach involves providing mental health resources alongside primary healthcare services, ensuring that individuals receive well-rounded support.
Moreover, cultivating global health partnerships is essential for advancing universal healthcare. Collaboration among nations, non-profit organizations, and private sectors fosters the sharing of knowledge, resources, and best practices. Such partnerships can effectively address common health challenges and enhance the resilience of health systems worldwide. While challenges in universal healthcare persist, these innovative trends present pathways for enhancement, aiming to create sustainable and equitable health systems across the globe.