In the realm of modern science, few innovations have sparked as much excitement and promise as CRISPR. This gene-editing technology, often likened to molecular scissors, allows scientists to precisely cut, edit, and replace segments of DNA. Since its emergence in the early 2010s, CRISPR has evolved from a bacterial defense mechanism into a transformative tool reshaping medical treatments. As of 2025, it stands at the forefront of a revolution in medicine, offering hope for curing genetic diseases, combating cancer, and tackling infectious illnesses like HIV. This article explores how CRISPR is fundamentally altering the landscape of healthcare, from groundbreaking clinical trials to personalized therapies tailored for individual patients.
A Brief History of CRISPR’s Rise
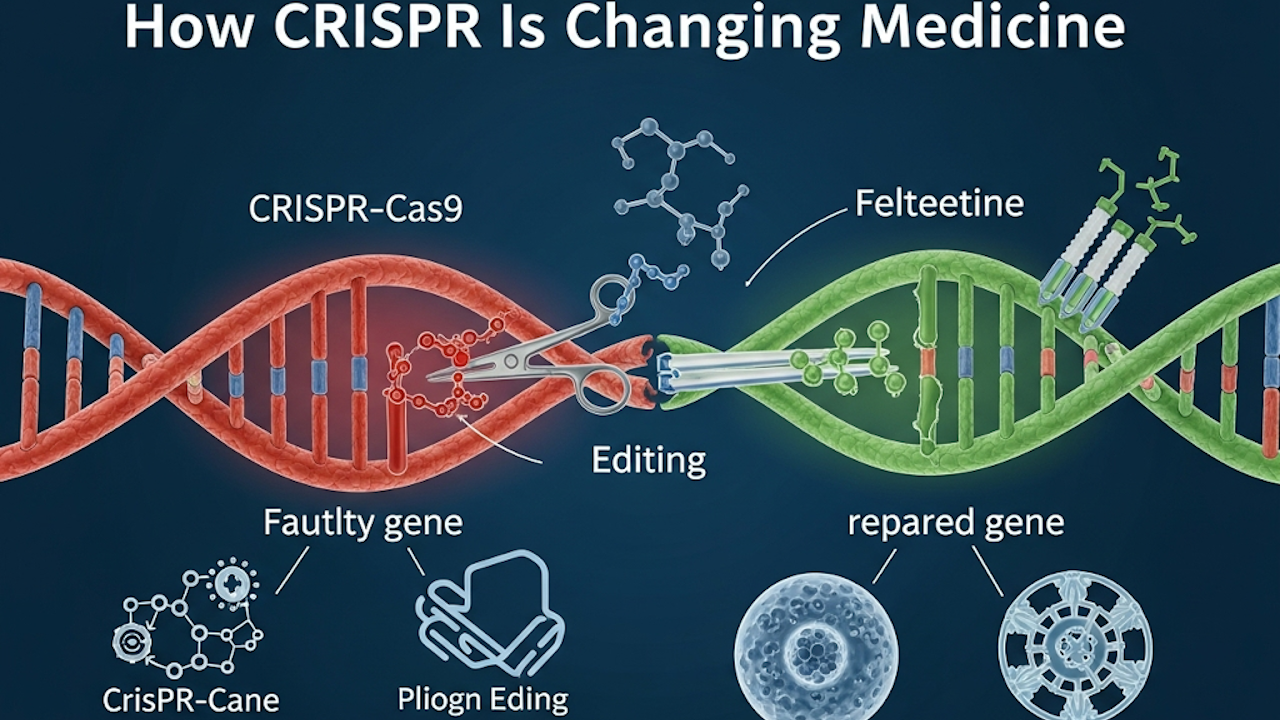
CRISPR, short for Clustered Regularly Interspaced Short Palindromic Repeats, was first identified in bacteria as a way to fend off viral attacks. In 2012, scientists Jennifer Doudna and Emmanuelle Charpentier harnessed this system, pairing it with the Cas9 enzyme to create a programmable tool for editing genomes. Their work earned them the Nobel Prize in Chemistry in 2020 and ignited a global race to apply CRISPR in medicine.
Early applications focused on basic research, but by the late 2010s, the technology entered human trials. The pivotal moment came in December 2023, when the U.S. Food and Drug Administration approved Casgevy, the first CRISPR-based therapy. Developed by CRISPR Therapeutics and Vertex Pharmaceuticals, Casgevy treats sickle cell disease and transfusion-dependent beta thalassemia by editing patients’ stem cells to produce functional hemoglobin. By 2025, this therapy has expanded to over 50 treatment sites across North America, the European Union, and the Middle East, with ongoing efforts to secure reimbursement from programs like U.S. state Medicaid and the UK’s National Health Service. This approval marked not just a scientific milestone but a proof of concept: gene editing could become a standard medical intervention.
The Expanding Landscape of Clinical Trials
Fast forward to 2025, and CRISPR’s impact is evident in the sheer scale of clinical research. As of February, approximately 250 trials involving gene-editing candidates are underway worldwide, with more than 150 actively recruiting participants. These span Phase I safety assessments to Phase III efficacy evaluations, covering a broad spectrum of conditions. Blood disorders remain the frontrunner, with numerous Phase III trials targeting sickle cell disease and beta thalassemia. For instance, studies like NCT03167450 and NCT03745287 are refining delivery methods and long-term outcomes for these hemoglobinopathies.
Cancer trials form another major pillar, addressing both blood and solid tumors. In hematological malignancies, trials such as NCT05066165 for acute myeloid leukemia and NCT04213469 for B-cell non-Hodgkin lymphoma use CRISPR to engineer immune cells that better attack cancer. Solid tumors are not left behind; efforts include NCT05812326 for breast cancer and NCT03525782 for non-small cell lung cancer, where edited T-cells target tumor-specific antigens. Rare diseases round out the portfolio, with trials for conditions like Leber congenital amaurosis (NCT03872479), Duchenne muscular dystrophy (NCT05514249), and phenylketonuria (NCT04768348). These initiatives leverage not just CRISPR-Cas9 but advanced variants like base editors and prime editors for finer control over genetic changes.
The diversity of these trials underscores CRISPR’s versatility. Early phases prioritize safety, testing dosages in small groups, while later stages measure real-world benefits. A comprehensive tracker at CRISPR Medicine News highlights how these efforts are accelerating, with new enrollments surging in 2025 despite economic headwinds.
Personalized Therapies: A Game-Changer for Rare Diseases
One of the most profound shifts CRISPR brings to medicine is the advent of personalized treatments. In a landmark case from early 2025, Children’s Hospital of Philadelphia (CHOP) administered the world’s first bespoke CRISPR therapy to an infant named KJ, who suffered from severe carbamoyl phosphate synthetase 1 (CPS1) deficiency. This ultra-rare metabolic disorder impairs the liver’s ability to process ammonia, leading to toxic buildup that can cause brain damage or death.
KJ’s treatment, developed in collaboration with Penn Medicine, was a feat of speed and precision. Starting in 2023, researchers identified KJ’s specific genetic mutation and designed a custom CRISPR payload to correct it. Delivered via lipid nanoparticles directly to the liver, the therapy was infused in February 2025, when KJ was just six months old, followed by boosters in March and April. The process, from diagnosis to first dose, took only six months, showcasing CRISPR’s potential for rapid customization.
Early results are encouraging. KJ now tolerates a higher-protein diet, relies less on nitrogen-scavenging drugs, and has bounced back from common childhood viruses without ammonia spikes. No serious side effects have emerged, though long-term monitoring continues. Published in The New England Journal of Medicine, this case paves the way for “platform therapies” that regulators can approve swiftly for similar rare disorders, bypassing lengthy traditional trials. For families facing untreatable conditions, where options like liver transplants are risky for infants, CRISPR offers a lifeline. This approach could extend to thousands of rare genetic diseases, democratizing access to cutting-edge care.
Targeting Blood Disorders: From Approval to Expansion
Blood disorders were CRISPR’s entry point into approved therapies, and 2025 has seen further consolidation. Casgevy’s rollout continues to refine patient selection and manufacturing, with positive early data from heart disease trials also emerging. Companies like Verve Therapeutics, focused on cardiovascular applications, were acquired by Eli Lilly in June 2025 to accelerate in vivo editing for conditions like high cholesterol. These ex vivo strategies, where cells are edited outside the body and reinfused, have proven safe and effective, but in vivo methods, which edit genes directly in patients, promise simpler administration.
Revolutionizing Cancer Treatment
Cancer remains a prime target for CRISPR’s immune-boosting capabilities. Allogeneic CAR-T cell therapies, derived from healthy donors rather than patients, are gaining traction to make treatments more scalable and affordable. CRISPR Therapeutics’ CTX110 and CTX130, for example, knock out immune-rejection genes while inserting cancer-targeting receptors, showing promise in trials for lymphomas and renal cell carcinoma (NCT04035434, NCT04502446).
Caribou Biosciences’ CB-010 stands out, combining CD19 targeting with PD-1 knockout to combat T-cell exhaustion. In the Phase I ANTLER trial (NCT04637763), it achieved a 94 percent overall response rate in B-cell non-Hodgkin lymphoma patients. Base editing variants, like those inactivating CD52 and TCR genes in CAR7 T-cells, have induced remission in pediatric leukemia cases (NCT04557436). PACT Pharma’s personalized TCR insertion trial (NCT03525782) stabilized disease in metastatic solid tumors for several participants.
These innovations address key hurdles in traditional CAR-T therapy, such as limited persistence and cytokine storms. Yet, challenges persist: off-target edits, Cas9 protein immunogenicity, and risks like secondary malignancies require vigilant monitoring. Ongoing refinements, including epitope masking and cytokine knockouts, aim to enhance safety.
Neurological Breakthroughs: Repairing the Brain
Neurodegenerative diseases, long considered untreatable, are entering CRISPR’s crosshairs. In May 2025, Stanford researchers unveiled CRISPR-TO, a Cas13-based system that shuttles RNA to damaged neurons without altering DNA. Targeting amyotrophic lateral sclerosis (ALS) and spinal muscular atrophy, where faulty RNA transport halts nerve repair, CRISPR-TO uses “address” signals to deliver repair molecules precisely. In mouse models, it boosted neurite growth by up to 50 percent in 24 hours, identifying RNA candidates for human trials.
This non-genomic approach sidesteps ethical concerns around heritable changes and could extend to traumatic brain injuries. Funded by the National Institutes of Health, the technology’s publication in Nature signals a shift toward RNA therapeutics for brain health.
Battling HIV: Toward a Functional Cure
HIV therapy via CRISPR focuses on excising viral DNA from reservoirs. Excision BioTherapeutics’ EBT-101, delivered by AAV9 vectors, targets three HIV genome sites to prevent viral rebound. The Phase I/II trial (NCT05144386), fast-tracked by the FDA, dosed its first patient in 2022 and reported no adverse events at 48 weeks in early participants. While a full cure remains elusive due to HIV’s mutations, combining CRISPR with antiretrovirals shows potential for long-term suppression.
CCR5 knockout strategies, rendering cells resistant to infection, continue in trials like NCT03164135. Edited B-cells producing neutralizing antibodies have protected mice from infection, hinting at multilevel defenses.
Cutting-Edge Tools Enhancing Precision
Beyond applications, 2025 has brought tool refinements. Yale’s CRISPR-Cas12a enables multiplex editing, assessing multiple gene interactions in immune responses to cancers and autoimmune diseases. By creating Cas12a mouse lines, researchers model complex disorders like liver disease and lung cancer more accurately, accelerating therapy development. Published in Nature Biomedical Engineering, this tool promises broader insights into genetic networks.
CRISPR Therapeutics’ 2025 collaboration with Sirius Therapeutics targets RNA interference for liver diseases, blending gene editing with silencing techniques. Such synergies highlight the field’s maturation.
Challenges on the Horizon
Despite triumphs, CRISPR faces obstacles. Financial strains, including biotech layoffs and a proposed 40 percent cut to NIH funding in early 2025, threaten progress. High costs and off-target risks demand rigorous safeguards. Ethical debates around germline editing persist, though somatic (non-heritable) applications dominate clinical work.
The Road Ahead
Looking to 2030 and beyond, CRISPR could eradicate many monogenic diseases and personalize oncology. Conferences like the 2nd Annual CRISPR Medicine in Copenhagen (April 2025) foster collaboration, featuring virtual sessions on innovative therapies. With over 250 trials in motion, the pace suggests dozens of approvals by decade’s end.
Conclusion
CRISPR is not merely changing medicine; it is redefining what healing means. From KJ’s personalized cure to CAR-T assaults on cancer, this technology empowers precision at the genetic level. As trials proliferate and tools evolve, patients stand to benefit from safer, faster paths to recovery. The journey is fraught with hurdles, but the potential to rewrite disease’s script makes CRISPR an enduring beacon of hope in 2025 and beyond.